The project seeks to design patient rooms for IU Health that better meet the needs of and improve safety for both patients and staff. IU Health is the largest network of physicians in the state of Indiana, offering a unique partnership with Indiana University School of Medicine, one of the nation’s leading medical schools. Project period: 2022-2023
Center for Health Facilities Design and Testing
View list of Awards
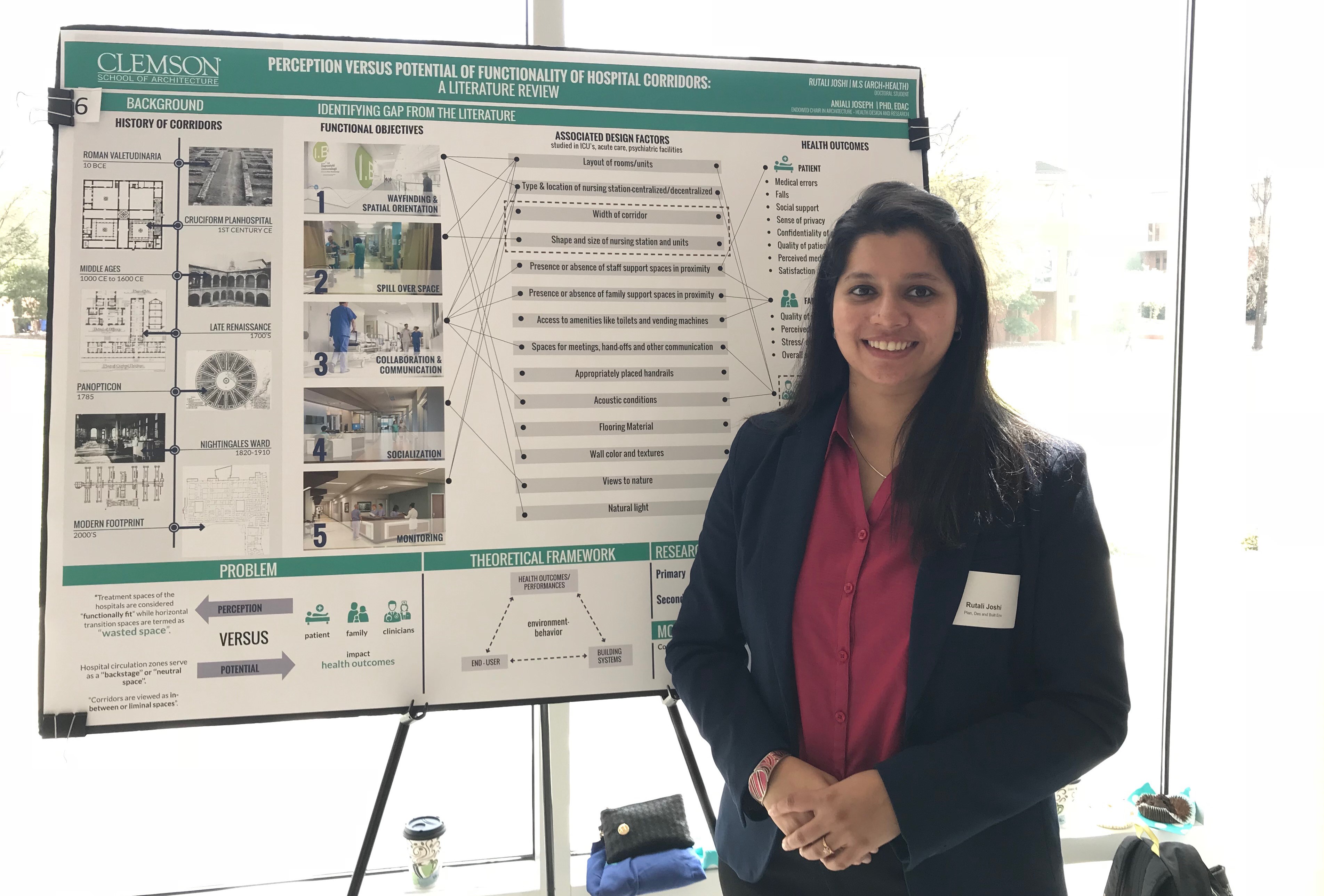
EDRA Best Student Poster Award | 2020
Rutali Joshi’s poster titled “Reduce Interruptions and Support Collaboration: Can the Workstation Design Support Physician Handovers in the Emergency Department?” has been awarded first place in the EDRA Best Student Poster category in April 2020. The award recognizes research that advances and disseminates behavior and design research toward improving understanding of the relationships between people and their environments.
ACHA Lifetime Achievement Award | 2019
David Allison, FAIA, FACHA, has received two national honors as a leader in health care design and architecture. The American College of Healthcare Architects has conferred its highest honor upon Allison, the ACHA Lifetime Achievement Award. The award, bestowed by fellow ACHA board members and past presidents, recognizes Allison’s full body of work in the field and his lasting influence on the theory and practice of health care architecture. Allison will be presented the ACHA Lifetime Achievement Award Nov. 3 in New Orleans at a luncheon being held in conjunction with the Healthcare Design19 Conference.
Healthcare Design Magazine | 2018
Dr. Anjali Joseph was the winner of the Healthcare Design Magazine research category for HCD 10, honoring professionals in different categories in the healthcare design field for their accomplishments over the past year.
Journal of Interior Design Excellence in Scholarship Award | 2018
Dr. Anjali Joseph received Journal of Interior Design Excellence in Scholarship Award at the Interior Design Educator’s Council for the paper titled, “Developing Evidence-based Tools for Designing and Evaluating Hospital Inpatient Rooms.
Institute for Patient Centered Design’s Outstanding Service Award | 2018
Dr. Deborah Wingler was awarded the Institute for Patient Centered Design’s Outstanding Service Award for her efforts as a patient and family advocate for healthcare design.
Frankie O. Felder Graduate Student Award of Excellence | 2018
Dr. Deborah Wingler was awarded the Frankie O. Felder Graduate Student Award of Excellence from Clemson University for her doctoral work.
American Academy of Healthcare Interiors Graduate Research Fellowship | 2017-2018
Dr. Deborah Wingler was awarded The American Academy of Healthcare Interiors Graduate Research Fellowship for her doctoral work.
Graduate Research and Discovery Symposium (GRADS) | 2018
Rutali Joshi
Rutali Joshi won 3rd place in Graduate Research and Discovery Symposium for her work in “Perception versus potential functionality of corridors.”This follows her award for 2nd place in the 2017 GRADS poster competition for her work in “Understanding the built environment of shelter homes for survivors of domestic violence.”
2017
Healthcare Design Expo + Conference, Orlando, Florida | 2017
Clemson’s University’s Architecture + Health program received numerous awards and recognition during this year’s Healthcare Design Expo + Conference in Orlando, FL. In addition to the awards below, a number of notable professors and students presented their research and findings at this year’s conference. Presenters: David Allison, Dr. Anjali Joseph, Byron Edwards, Dr. Dina Battisto, Dr. Susan O’Hara, Dr. Sara Bayramzadeh, Deborah Wingler, Chris Kiss, Will Lewis.
RIPCHD.OR
Realizing Improved Patient Care Through Human-Centered Design in the Operating Room (RIPCHD.OR) prototype was the solo winner in the conceptual design category for The Healthcare Environment Awards. The project also received Gold Level EBD for the Touchstone Awards, which recognizes the use of an evidence-based design process in the pursuit of increasing value, improving outcomes and engaging stakeholders.
Click to view project
Deborah Wingler
Deborah Wingler was honored with The Center for Health Designs Research Coalition’s New Investigator Award (NIA) which supports highly qualified research initiatives in evidence-based design (EBD).
Long-Term Acute Care Hospital
Austin Ferguson, a recent graduate from the Master of Architecture + Health program was The Healthcare Environment Awards winner under the student category for his Long-Term Acute-Care Hospital, which he designed as his comprehensive project.
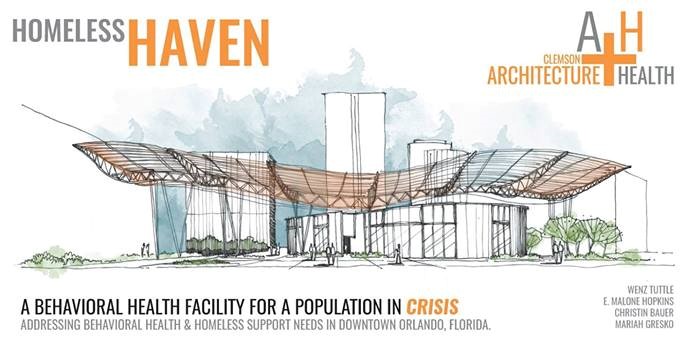
AIA-AAH STERIS Student Design Charrette,”Homeless Haven”
Malone Hopkins, Wenz Tuttle, Mariah Gresko, Christin Bauer, from the Master of Architecture + Health program, were selected to participate in the 2017 annual AIA-AAH STERIS Student Design Charrette with David Allison as their project advisor. The 48-hour project, a Behavioral Health Facility and Resource Center titled “Homeless Haven”, received the highest praise from the jury of professionals.
News Archive 2017-2020
Dr. Anjali Joseph delivers virtual presentation for the Columbia Museum of Art’s ArtBreak Series
Dr. Anjali Joseph, Director of the Center for Health Facilities Design and Testing (CHFDT), presented “Architecture and the Choreography of Healthcare” for the Columbia Museum of Art’s ArtBreak series. The virtual presentation, delivered on August 25th, provided examples of healthcare environments from observational studies to illustrate the dynamic interactions between the built environment, care providers and those receiving care, tasks performed, and the tools and equipment used. Dr. Joseph’s presentation demonstrated the importance of understanding these complex interactions when designing human-centered healthcare environments.
Dr. Anjali Joseph led a panel presentation at the virtual Human Factors and Ergonomics Society Healthcare Conference
Dr. Anjali Joseph led the panel presentation titled ‘Using simulation-based evaluations of physical and virtual mock-ups to design safer hospital environments’ at the virtual Human Factors and Ergonomics Society Healthcare conference May 18-20, 2020. The conference was originally scheduled to take place in Toronto on March 8-10. Dr. Joseph co-presented with speakers from the Children’s Healthcare of Atlanta and Health Quality Council of Alberta, Canada.
Dr. Anjali Joseph participated in an Agency for Healthcare Research and Quality review panel February 19-20 in Washington, D.C.
The group met to review grant proposals related to identifying risks and hazards that lead to medical errors and identifying solutions to prevent patient injury associated with the delivery of health care. The research findings and products include providing information on the scope and impact of medical errors on costs, quality, efficiency, and effectiveness of care; quality improvement research; examining and improving medical liability; identifying the root causes of threats to patient safety; research focused on healthcare associated infections; and examining effective ways to make system-level changes to help prevent errors and harms.
Architecture + Health program director David Allison receives lifetime achievement and Changemaker awards. Clemson website. September 10, 2019.
Rethinking the OR: Simulation Tests Researchers’ Ideas for Improving Operating Room Design. Clemson website. January 7, 2019
Rethinking the OR: Simulation tests researchers’ ideas for improving operating room design. December 17, 2018.
https://web.musc.edu/about/news-center/2018/12/17/or-of-the-future
Designing a Safer OR. Healthcare Design Magazine. November 16, 2018.
https://www.healthcaredesignmagazine.com/trends/research-theory/designing-a-safer-or/
Hospitals Look to Innovation to Inspire Design. HealthTech. October 22, 2018.
https://healthtechmagazine.net/article/2018/10/hospitals-look-innovation-inspire-design
How a patient advocate becomes a healthcare designer of the future. Clemson website. August 6, 2018.
Clemson professor named ’18 research-winner by Healthcare Design Magazine. Clemson website. August 2, 2018.
Inside the OR of the future: X-ray vision, ‘Siri for Surgeons,’ and more. May 31, 2018.
https://www.advisory.com/daily-briefing/2018/05/31/or-of-the-future
The Operating Room of the Future. The Wall Street Journal. May 28, 2018 by Laura Landro
https://www.wsj.com/articles/the-operating-room-of-the-future-1527559862
It’s Time to Build a Better OR. Outpatient Surgery Magazine (Special Edition). March, 2018 by Dr. Scott Reeves
Reimaging and reinventing surgical workspaces. Outpatient Surgery Magazine (Special Edition). March, 2018 by Dr. Anjali Joseph (pp 64-65)
Clemson, MUSC unveil operating room prototype. Charleston Business Journal. March 13, 2018
New operating rooms: S.C. researchers focus on changing antiquated design. KPVI 6. February 18, 2018
New operating rooms: S.C. researchers focus on changing antiquated design. Telezkope. February 18, 2018
New operating rooms: S.C. researchers focus on changing antiquated design. The Times and Democrat. February 18, 2018
Clemson, MUSC share gains made in OR design project. Clemson website. January 25, 2018 by Tara Romanella
MUSC, Clemson share gains made in OR design project. upstatebizSC. January 29, 2018 by Tara Romanella
Clemson architecture program teams up with MUSC to design a better operating room. The Post and Courier. January 29, 2018 by Lauren Sausser
Clemson project recognized for conceptual design excellence at Healthcare Design Expo. Clemson website. November 14, 2017 by Tara Romanella
MUSC, Clemson University collaborate in integrated OR suite designs. MUSC Catalyst News. August 29, 2017 by Olivia Franzese
http://academicdepartments.musc.edu/newscenter/2017a/integrated-OR-design2/
Realizing Improved Patient Care through Human-Centered Design in the Operating Room (RIPCHD.OR)
The Realizing Improved Patient Care through Human-Centered Design in the Operating Room (RIPCHD.OR) learning lab uses a socio-technical approach incorporating human factors engineering and evidence-based design principles to create an optimal ergonomically sound operating room that results in improved patient and staff safety. A multidisciplinary team comprised of human factors and industrial engineers, architects, environment and behavior researchers, medical equipment planners, anesthesiologists, nurses and quality and patient safety experts from Clemson University and the Medical University of South Carolina (MUSC) have worked collaboratively to develop, test (through iterative design cycles), implement and evaluate various OR design solutions. Some of the concepts developed as part of this learning lab are being implemented in two new ambulatory surgery centers built at the Medical University of South Carolina (MUSC) in Charleston.
Sponsor: Agency for Healthcare Research Quality
Project period: 2015 to 2020
Three highly interrelated and integrated patient safety focused projects related to key aspects of OR suite design have been undertaken over the course of the RIPCHD.OR project
Project 1: Unmasking of anesthesia-related alarms and communications This work extends what is known about alarms, interruptions, and distractions in the operating room by examining them from a systems perspective. Project 1 involves several phases with the goals of: 1) developing and evaluating systems design methods that account for masking affect tasks within the OR environment and 2) exploring interface design as a means to mitigate the effects of masking.
Project 2: Traffic flow and door openings in the OR This project focuses on understanding factors impacting traffic flow in the OR suite. Using a systems approach, the flow of supplies, equipment, information and people in the OR is being studied and the factors impacting traffic flow and distribution are being analyzed to develop solutions that minimize door openings and flow disruptions in the OR.
Project 3: Integrated OR suite design This project provides the overall framework for integrating the work of this learning lab. This project is developing an overall framework and methodology for designing an ergonomic and human-centered operating room that will improve patient and staff safety and outcomes in the OR. The project team for OR suite design has worked closely with the other project cores to determine optimum procedure room configuration, orientation and intra-room zoning that supports the performance of the surgical team, improves workflow within the team, enhances visibility of work and team members, minimizes distractions of team members and reduces risk of surgical site infections.
AIM 1: Formally structure the RIPCHD OR learning lab and establish laboratory infrastructure and team management.
AIM 2: Develop a systematic approach to evaluating the impact of people, tasks, tools and technology and the built environment in developing ergonomic and human-centered operating room design solutions.
AIM 3: Develop evidence and recommendations related to the use of advanced displays and multimodal displays for anesthesia tasks to mitigate the masking of important signals.
AIM 4: Develop process design recommendations to support key OR flows (OR team members, supplies, patient, equipment, information) that impact patient safety outcomes such as surgical site infections and surgical errors.
AIM 5: Develop an evidence-based framework and methodology for designing operating rooms that achieve the desired patient and staff safety outcomes.
Designing Preoperative and Post-operative Workspaces
The collaborative project, funded by a gift from Haworth through the Watt Family Innovation Center, explores preoperative and postoperative workspaces within complex ambulatory surgery centers (ASC). The spatial layout, furniture, and equipment of these work spaces should support patient, care partner and staff experiences within the context of emerging technologies and models of care. Multiple studies over the course of the project have examined a human centered approach to designing preoperative and post-operative spaces in ASCs.
Sponsor: Gift through the Watt Family Innovation Center from Haworth
Project period: 2015 – 2018
Study 1: Observational study of preoperative and postoperative work spaces- This observational study used a multimethod approach consisting of in-depth literature review, behavior mapping, shadowing, spatial analysis, and semi-structured interviews with nursing staff to understand the work patterns of nurses in preoperative and post-operative workspaces of ambulatory surgery centers. This study identified environmental design strategies that support or act as barriers to critical interactions between care teams (care providers, patients and care partners) and addressed the emerging role of technology in ambulatory surgery workspaces as well as issues associated with integrating technology into existing workspaces.
Study 2: Development and application of ergonomic assessment tool- This study involved the development of an ergonomic evaluation framework and design tool that focused on the work system versus the workstation in preoperative and postoperative workspaces in ASCs. As part of this study, the tool was tested and refined across several facilities with varying spatial configurations and workstation types.
Study 3: Comparing design alternatives using virtual reality- This study involved designing and testing innovative solutions of pre/postoperative rooms addressing a range of design and performance goals including the integration of a computer workstation to support electronic charting. Architecture + Health studio (class of 2018) participated in a two-week design intensive to develop and design three distinct prototypes of pre/postoperative rooms with varying types of workstations integrated into their work system. Each of these prototypes were evaluated by nurses using virtual reality to understand how well user goals were met. From these three prototypes, one was chosen and modified to incorporate the findings from the evaluation. This new prototype will be tested for its functional capabilities with users in a full-scale cardboard mock-up.
Designing Waiting Rooms in Surgical Environments
Waiting rooms in healthcare environments have been previously studied to understand how factors such as aesthetics, privacy, comfort and incorporation of positive distractions impact user perception of quality of care. Though care partners of patients undergoing surgery often spend long hours in the surgical waiting rooms, no studies have examined how the built environment including the layout of the waiting area and design of seating could support their waiting experience.
Sponsor: Gift through the Watt Family Innovation Center from Haworth
Project period: 2018 to 2020
This study determines how furniture location impact care partners’ choice of seating in a virtual outpatient surgery waiting area during various tasks including patient check-in, receiving a phone call, getting coffee, and waiting for surgery to end. A multimethod approach including a survey and semi-structured interviews was utilized to capture participants’ seat selections as well as their feedback on how certain factors (e.g., visibility, accessibility, privacy, comfort, and aesthetic quality) impacted their choices. Additionally, the researchers obtained feedback on usability, comfort and aesthetic quality of seating furniture products that were incorporated in the virtual environment.
CU@HOME: Developing a technology-based intervention to assess the home and community environment to prevent falls in the home and support aging in place.
The purpose of CU@Home is to understand the feasibility of using a technology-based intervention to proactively assess the home and community environment of older adults scheduled for joint replacement surgeries. The feasibility study is conducting an in-depth literature review; a series of interviews and focus groups with key stakeholders (primary care physicians and clinical staff, discharge planners, home health nurses, patients and families) to clearly understand all aspects of the problem; and to explore potential data needs, data sources, and technological solutions required to develop this intervention.
Sponsor: Clemson Faculty Research Development Program
Project period: 2019 to 2020
The overall broader research plan of this multidisciplinary team is to develop a technology-based intervention that could be used prior to joint replacement surgeries to help older adults evaluate their own homes for safety risks and to identify resources in their community to support home modifications. We envision that this tool would support both the clinical team as well as the older adult and their families in coming up with built environment solutions that would prevent falls and support their care needs. The tool would also help the patient access resources in their community to enable home modifications and to support safe recovery post-surgery. We also envision that this tool would be connected to the patient’s health record or patient portal such that this data will be available to other care teams that interact with the patient at different stages (e.g. a hospital discharge planner who may need to need to know key characteristics of the home while transitioning a patient back after a hospital stay).
Identifying and Reducing Errors in Perioperative Anesthesia Medication Delivery (OR SMART)
The major goal of Identifying and Reducing Errors in Perioperative Anesthesia Medication Delivery (OR SMART) is to engineer reductions in anesthesia medication errors in operating rooms. This study uses a systems’ engineering approach to improve decision making, reduce procedural and technological vulnerabilities and improve the work environment and culture. A highly experienced multi-disciplinary team of clinicians, scientists and engineers is using a combination of innovative techniques to address this threat to patient safety in the most comprehensive study of anesthesia medication safety systems ever conducted.
Sponsor: Agency for Healthcare Research Quality
Project period: 2018 – 2021
AIM 1. Explore Solutions to Failures in Diagnosis, Selection and Prescribing of Intraoperative Anesthesia Medication.
AIM 2: Develop methods to reduce failures in the preparation, administration and recording of intraoperative anesthesia medication
AIM 3: Understand and improve workspace design and safety culture to influences anesthesia medication selection and delivery.
Human Factors Considerations in the Design and Implementation of Telemedicine-Integrated Ambulance-based Environments for Stroke Care
This collaborative project examines the process flow, workload and usability issues associated with ambulance-based telemedicine to evaluate and provide the requisite treatment to stroke patients in transit to the hospital. The goal is to understand the cognitive, physical and temporal demands placed upon caregiving teams in geographically dispersed remote locations, and to evaluate the potential for user/design errors that characterize the use of Information Technology (IT) systems in high-stress environments.
Sponsor: Agency for Healthcare Research Quality
Project period: 2019 – 2020
AIM 1. Evaluate the demands placed on the caregivers, the usability of the telemedicine system, and the barriers in the workflow associated in a telemedicine-integrated, ambulance-based setting for stroke care using the SEIPS 2.0 framework.
AIM 2: Iteratively develop and refine guidelines and recommendations for large-scale implementation of telemedicine systems for stroke care in ambulances.
The project seeks to develop guidelines for a system that can efficiently integrate telemedicine systems on ambulances to enhance caregiver-telemedicine system interaction and streamline workflow without increasing the physical, cognitive and/or temporal workloads on the stakeholders who use these systems.
Systems Evaluation of Pediatric Intensive Care Unit Rooms
The simulation team at Children’s Healthcare of Atlanta has conducted several simulation-based evaluations of physical mock-ups as part of the design process for a new 400-bed freestanding children’s hospital. These simulations have highlighted the specific human factors and workflow challenges posed by room design, especially in critical high-risk situations. The purpose of this project is to focus on one particular high-risk patient care environment – the pediatric intensive care unit (PICU) room. This study utilizes videos of simulations conducted in high-fidelity physical mock-ups of PICU:
1. To conduct a systems evaluation of the PICU room in the context of multiple scenarios associated with a high-risk patient.
2. To simulate observed workflows and disruptions in a mirrored PICU room to identify design challenges and potential solutions
Sponsor: Children’s Healthcare of Atlanta
Project period: 2020